•Nigeria now manufactures 45% of drugs need owing to massive scale up post COVID 19 pandemic, says PMGMAN
•To attain self sufficiency, PMGMAN calls for declaration of emergency on local pharmaceutical manufacturing sector
•Recommends high-powered task team to look at medicines security approach adopted by India, China
It is feared that Nigeria is at the mercy of Western and Asian countries, as ‘unreliable’ sources of her essential drug needs. Some unconfirmed reports indicate that only 30 per cent of drugs used in Nigeria are produced locally and the country depends on China and India for the remaining 70 per cent.
Studies have shown that Nigeria and other African countries spend at least $14 billion on importation of pharmaceutical products needed in the continent. It is very frustrating to see the products, which the pharmaceutical industry has the capacity and competence to produce locally, being imported into the Nigerian market.
Drug security is defined as measures put in place to ensure that quality, safe and efficacious and sufficient medicines are produced by facilities that meet the right standards and, that the integrity of such medicines are not compromised during its distribution along the supply chain from the manufacturers down to the consumers.
The imperative of national drug security is enshrined in the National Drug Policy, which is to make available at all times to the Nigerian populace adequate supply of drugs that are effective, affordable, safe and of good quality; to ensure the rational use of such drugs and to stimulate increased local production of such drugs.
The Sustainable Development Goal (SDG) goal number 3 speaks to good health and wellbeing with one of its targets being Universal Health Coverage (UHC), access to quality essential healthcare services and access to safe, effective, quality and affordable essential medicines and vaccines for all.
Recently, at the State House Medical Centre in Abuja, there was an alleged incident of non-availability of drugs and medical devices; the case at a primary healthcare centre in a rural area is worse. The reality of drug security in Nigeria can be dire; many times it is disease- or population target-based. According to the report of the Federal Ministry of Health, drugs used for diabetes or cancer cost two-day wage or five times the monthly wage of a minimum wage worker respectively. This is exacerbated if the patient is at the low-income level, where 62 per cent of Nigerians belong.
Several studies have shown that Substandard and Falsified Medicines (SF) low-priced drugs have contributed greatly to drug insecurity in Nigeria. The public health implications of substandard and falsified medical products are serious and critical. The outcomes include treatment failure, high treatment cost, and development of resistance. This may ultimately result in fatality and loss of confidence in the healthcare providers and healthcare system.
At the peak of COVID-19 pandemic in 2020, countries like India banned the export of essential drugs, Active Pharmaceutical Ingredients (APIs) and other critical pharmaceutical products.
Recently, the British Government banned the export of antibiotics used to treat potentially deadly Strep A infections amid claims of a shortage.
According to reports, pharmacies in the UK had run out of stock and the price wholesalers were charging for the bug-busting drugs had surged five-fold following deaths of at least 16 children.
The antibiotics were added to a list of medicines that cannot be exported amid shortage fears. They are amoxicillin, cefalexin, phenoxymethylpenicillin (Penicillin V) and azithromycin oral suspension.
The situation has raised the question: How self-sustaining is Nigeria’s capacity to be self-sufficient in drug production?
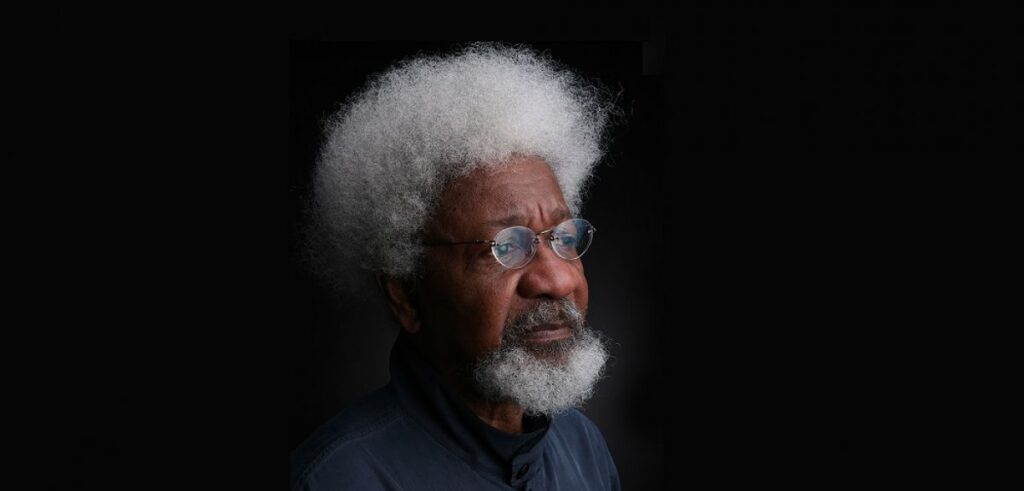
Chairman, Pharmaceutical Manufacturers Group of Manufacturers Association of Nigeria (PMGMAN), Dr. Fidelis Ayebae, told The Guardian that PMGMAN is working on getting the right data and it will bring peoples attention to it, when validated.
PMGMAN represents all the manufacturers of pharmaceuticals and allied products in Nigeria, who collectively play key role in ensuring that Nigerians have timely access to affordable, safe and high quality medicines, as well as contribute to national development.
Ayebae said the production has been scaled up to 45 per cent of her drugs need are being manufactured locally, and this is one of the takeaways, the silver lining that came with the pandemic as state governments and development partners helped in the post-COVID 19 recovery.
Ayebae, who is also the Chief Executive Officer (CEO) and Managing Director of Fidson Healthcare Plc., said the only strategy to build a resilient and agile supply chain of essential medicines in the country is to manufacture these life-saving products domestically.
“This aligns with our Medicines Security (MS) goal – it is the only most sustainable strategy indeed,” he said.
The Fidson boss said, today, the local pharmaceutical industry through Public Private Partnership (PPP) with states are playing key role closing the gap in supply chain of medicines at state level.
“Thanks to African Resource Centre for Excellence (ARC-ESM) Bill and Melinda Gate foundation support, for brokering these partnership and believing in the capacity of local pharmaceutical industry in Nigeria,” he said.
According to him, Kaduna, Niger, Nassarawa, Sokoto, Ekiti, and Yobe have attained milestones. He said they are in strong partnership buying locally manufactured medicines and the same with some donor organisations. With these partnerships in some states, out of stock is being reduced to an insignificant number.
“We can’t thank these states enough for leading in this disruptive model, that will not only guarantee access to safe, quality and affordable medicines, but also will translate to economic development for Nigeria and capacity building for the local pharmaceutical industry,” Ayebae said.
According to him, if only governments can join forces and walk the talk of – following through faithfully on Executive Order 3 of Mr. President, National Drug Policy of buying 70 per cent locally, and convergence of all policies that speak to the sector, Nigeria will leapfrog and set the record straight as the next frontier for pharmaceutical manufacturing in Africa.
He further explained: “We can manufacture for Africa, we have the capacity. Before now, our facilities were under-utilised to almost 60 per cent, yet we, do have enormous capacity to produce these medicines in our facilities.
Next year, PMGMAN will attain 40 years of advocacy on MS, a concept that is a buzzword in the public space today. But for the records- PMGMAN conceptualised this as a document to bring the attention of the policymakers and government on the dangers of not prioritising and mainstreaming the local pharmaceutical sector, which we were vindicated in the wake of the pandemic.
“Have we learnt our lessons or we are still playing to the gallery, only time will tell, because we are all some years away from the next pandemic. Trust me, the consequences will be dire, if we don’t mainstream the local pharmaceutical to drive the country towards self sufficiency.”
On how to address the issue and achieve medicines security in Nigeria, Ayebae said: “Ours as a group is to innovate and repurpose our facilities to compete globally, within the context which the government policy allows. Of course, you and I are conversant with the many challenges – policies that are not followed through faithfully, the competition amongst regulators and gatekeepers on revenue drive that the manufacturer ends up being the victim and the discordant policies that add to high cost of production. Today, you pay close to 60 per cent cost of production on energy, the infrastructural deficit and the debt burden and so on. So, to get Nigeria to become self sufficient, the local pharmaceutical manufacturing is one sector that should be declared an emergency sector because of the peculiarity of the role they play.
“We need to start seeing attainment of medicine security concept, as designed by PMGMAN as an art of defence, diplomacy and development, just like other developing and developed countries like India, China, Bangladesh, that adopted – ‘A war foot approach’.
“Until you exert sufficient input on how the medicines you consume are produced in the country, access to safe, quality, and affordable medicines will continue to be rhetorical assertion,” he said.
Ayebae is concerned that the political/economic decision-making organ of government are not seeing the situation from the lens of National Security? He wondered why the Federal Government, set up a health Reform committee and didn’t deem it fit for manufacturers to be in the room to speak to these many bottlenecks that keep reversing efforts to be sufficient and free from import dependence.
Ayebae said: “Post COVID-19 India, the pharmacy capital of the world, led by the President set up a committee to ensure that never again, will they be dependent on China to get the active pharmaceutical Ingredient (API). They put up an incentive based scheme and empowered local pharmaceutical companies to achieve a set target in this regard. Approximately 75 per cent of API used in India comes from China and they learnt the hard lessons during the pandemic. Going forward, they don’t want such to repeat itself. That is forward thinking and we need to get to work and have a high-powered task team of PMGMAN and FG, to look at this from the war foot approach (National Security), adopted by these countries, which are already advanced in the pharmaceutical manufacturing space.
“We need to start from the low hanging fruit, we already have a robust local pharmaceutical space approximately 120 plus. I call them patriots, we must have an emergency taskforce on what I call policy convergence team made up of PMGMAN, Federal Ministry of Finance, Budget and National Planning (FMoFBNP), Federal Ministry of Industry Trade and Investment (FMITI) and Federal Ministry of Health (FMOH) to be driven by us, supported by the FG in a stewardship role. However, they must see the industry from the lens of national, economic and heath security to mainstream the sector for innovation, competition and attainment of self sufficiency status for Nigeria.”
National Chairman, Clinical Pharmacists Association Of Nigeria (CPAN), Dr. Joseph Madu, told The Guardian investigations by the country’s pharmaceutical bodies have shown that only about 20 to 30 per cent of drugs are manufactured locally, while about 70 to 80 per cent are imported from different countries including China and India.
Madu said the cause of the problem couldn’t be far-fetched as the country imports up to 90 per cent of her APIs and excipients. “We also import almost all the equipment used for manufacturing of drugs locally,” he said.
The pharmacist said a lot of other factors make it preferable for companies to import rather than manufacture locally. Such factors, he said, include lack of patronage of local companies by governments and donor agencies, high cost of production, high tariffs, high taxation and trade related barriers on importation of APIs, etc.
Madu said poverty and lack of education is another reason as many Nigerians enjoy getting cheap drugs from traders instead of quality drugs from registered pharmacies, which may be costlier. “Most cheap drugs are not manufactured locally and are mostly fake. Choosing cheap and likely low quality or fake drugs, from drug vendors affects patronage of locally manufactured products, which are mostly of higher quality and sometimes costlier,” he said.
The pharmacist further explained: “Finally, the pharmaceutical sector is a part of the larger economy, and whatever happens to the economy is bound to affect the sector.
“All problems of our economy such as poor infrastructure, poor power supply, corruption, insecurity of lives and property, which currently plague our economy, will definitely impact negatively on our Pharmaceutical manufacturing sector leading to the unacceptable level of medicines production in the country.”
On the hazards of heavy reliance on imports, the pharmacist said: “The security of the nation cannot be guaranteed. Take for instance, during the COVID-19 lockdown, if the situation had continued, it would have meant that a lot of Nigerians would have died, as there won’t be access to medicines to treat even common ailments.
“Also, dangerous and unsafe products can be manufactured elsewhere and imported into the country as medicines.
“Secondly, if you are producing your medicines in your country, your regulatory agencies can frequently visit the manufacturing companies to ensure compliance with the dictates of Good Manufacturing Practice (GMP) for medicines production. But this cannot be done for imported medicines.”
Madu said the dangers of depending on importation include, lack of capacity to create job and economic development opportunities, loss of revenue generation, lack of sustainable access to high quality medicines, and lack of national pride as a production country instead of a consumption country.
On why import substitution efforts have not worked, Madu said: “It has not worked because the government is yet to tackle some of the challenges enumerated above.
“Secondly, the government is yet to carry the relevant pharmaceutical associations and experts fully along, in the decision making process. For instance, when Nigeria signed the African Continental Free Trade Agreement (AFCFTA), I do not think that the Pharmaceutical Society of Nigeria (PSN) or PMGMAN was fully carried along, else it would not have been acceptable to them to impose some percentage of tariffs on importation of APIs.
“Most of the African countries that signed the agreement do not have a substantial number of local drug manufacturing companies. But Nigeria has almost up to 200 local manufacturing pharmaceutical companies.
“Furthermore, associations such as the Clinical Pharmacists Association of Nigeria can be fully engaged by the government as they help to bridge the gaps between drug manufacturers and promotion of direct patient centered care use of drugs by the population and other healthcare providers.”
On how Nigeria can achieve urgent self- sufficiency on medicines, Madu recommended that government should financially support local manufacturing companies to obtain World Health Organisation (WHO) pre-qualification certification. He said this certification costs huge amount of money to obtain, and without it the WHO, the United Nations (UN), and other donor agencies cannot patronise a local manufacturing company.
Madu said if governments support and encourage local pharmaceutical manufacturing companies to get the WHO pre-qualification certification, this could help to boost patronage and encourage local production.
The pharmacist said government should set up a committee to ensure the full implementation of the National Drug Policy 2021 to the letter. The policy also seeks to ensure that by year 2025, Nigeria will be able to achieve up to 75 per cent of local manufacturing of essential medicines.
Madu said, being the biggest buyer of medicines in the country, the government can deliberately create a policy to patronise local products. “They should only buy imported medicines in public hospitals, where there is no available locally manufactured alternative. This will invariably boost patronage of our local manufacturing pharmaceutical companies.
“Government can achieve this by signing an Executive Order in this regards.The current Executive Order of the government on imported products into Nigeria does not include pharmaceuticals,” he explained.
Madu said government should develop the petrochemical sector. According to him, substantial raw materials for synthetic medicines are got from the petrochemical industry. It is important to let the government know that Nigeria is blessed with petrochemicals, which can be engaged for production of APIs.
“With basic APIs, we can start producing a larger percentage of drugs locally. We have enough pharmacists and pharmaceutical manpower to take advantage of achieving the set goals,” Madu declared.
The clinical pharmacist said Nigeria should develop the agricultural sector. “For instance, starch is used in the production of many pharmaceutical drugs.
But Nigeria, however, has no pharmaceutical grade starch. Pharmaceutical grade starch can be developed from our local cassava, maize, corn etc. A lot of phyto-medicinal plants can be grown locally through boosting of agricultural sector.
Such plants can be used in the local manufacturing of phyto-medicines in the country,” he suggested. Immediate past Chairman, Association of Hospital Pharmacists of Nigeria (AHPN) and Deputy Director of Pharmaceutical Services, Federal Medical Centre, Asaba, Delta State, Dr. Kingsley Chiedu Amibor, told The Guardian that Nigeria depends heavily on imports for finished products and active pharmaceutical ingredients, as much as 70 per cent and majorly from China and India.
Amibor said this situation runs counter to the provisions of the National Drug Policy, which seeks to “make available at all times to the Nigerian populace adequate supply of drugs that are effective, affordable, safe and of good quality; to ensure the rational use of such drugs and to stimulate increased local production of such drugs.”
The pharmacist said rather than witnessing increase in local production of drugs, the reverse had been the case for quite some time. He said the pharmaceutical industry in Nigeria had been performing below capacity, and this was made worse during the COVID-19 pandemic.
Amibor said at some point, only about 30 per cent of adults and 20 per cent of children living with Human Immuno-deficiency Virus (HIV)/Acquired Immune Deficiency Syndrome (AIDS) had access to antiretroviral drugs, while some essential drugs for diabetes and cancer were only accessible at prohibitive costs, sometimes several times more than the monthly minimum wage.
The pharmacist said the issue of concern is lack of access to finance to set up appropriate infrastructure and good pharmaceutical quality management system, in line with the WHO pre-qualification standard and benchmark. He said there are at least 150 pharmaceutical manufacturing firms in Nigeria; serving over 200 million people and not all of them were able to benefit from the CBN’s N100 billion intervention fund. So, for some of them, Amibor said, lack of finance is still a challenge.
The pharmacist said public health institutions have also been on the receiving end of medicines insecurity, arising from inefficient storage, transportation and distribution facilities, poor selection and procurement practices, involvement of incompetent persons in procurement, distribution and sale of medicines, poor performance of drug suppliers, high cost of imported products and failure of the Drug Revolving Fund (DRF) scheme to sustain medicines availability in the health institutions. He said the result has been medicines shortage in these institutions with grave health consequences such as increased morbidity and mortality.
On the hazards of heavy reliance on imports, Amibor said one major consequence of reliance on imports is that Nigeria has now become a dumping ground for all manner of pharmaceutical products, which has a direct effect on the profitability of local industries. He said this scenario has exposed the country to dangers of falsified and substandard pharmaceutical products such as treatment failures, increased morbidity, high treatment cost, distribution of medicines of questionable quality, development of antimicrobial resistance and deaths.
On the failure of import substitution, Amibor said while import substitution is important, it is a very restrictive vision. It looks towards survival, instead of looking to create wealth through greater export market and value diversification. The result, he said is a manufacturing sector that cannot develop nor compete globally, but limits itself to survival mode, not a global manufacturing growth mode. Rather than being reactive, Nigeria would need to be proactive,” he added.
Amibor said import substitution failed for several reasons such as, lack of external competition in the import substitution industrialisation strategy, which meant that firms are not under competitive pressure to improve their products and technology, leading to obsolete products.
“Once the economy is forced to open up, these protected industries usually collapse under the relentless pressure of foreign competitors. Additionally, import substitution can impede growth through poor allocation of resources, and its effect on exchange rates harms exports,” he said.
On how Nigeria can achieve urgent self-sufficiency on medicines security, Amibor said for Nigeria to attain medicines security, there is need to promote, protect, grow the pharmaceutical industry. He said all hands must be on deck to achieve this objective, including the government.
Amibor urged the Federal Government to develop a sustainable and efficient local drug industry as a sine qua non for medicines security. He said this is expected to take decades of dedication by both the private sector and government.
He said government should complement the development of drug manufacturing by increasing financial support to the sector that will result in expansion of the manufacturing firms. This, he said, will go a long way to achieving medicines security.
Executive Secretary, PMGMAN, Frank Muonemeh, had told journalists: “We are aware that in the wake of COVID-19, globalisation is being threatened as countries are looking inwards for home grown solutions to their problems. According to International Trade Centre Market Access Map (www.macmap.org/covid19), as at June 18, 2020, 95 countries placed temporary export restrictions on the essential COVID-19 pharmaceutical and non pharmaceutical products used in response to COVID-19, inclusive of some African countries, hence the need for countries to look inwards for home-grown solutions. The fallout of this realisation is that every country looks inward for solutions.
“It is time we reverse the country’s over-dependence on imported medicines. It is time we focus on how to attain medicine security and national self-sufficiency, just like many other countries are on reset thinking, with globalisation being threatened by protectionism.”
Acting Director General of NAFDAC, Dr. Monica Eimunjeze, said the agency recognises and appreciates the need for drug security and continues to strengthen its regulatory processes with a fully functional regulatory framework. Eimunjeze said the Agency’s regulatory function is working toward stringent policies and at the same time guiding and enabling the local manufacturers in quality management and better productivity.
According to NAFDAC, from product development up until when the product reaches the patient – various structures of the Agency come into play – be they clinical trial oversight, laboratory analysis, ports inspection, narcotic control, chemical evaluation, pharmacovigilance, registration, GMP inspection, investigation and enforcement. All of these allow for continued compliance with legislative provisions and policies of government that ultimately result in drug security.
Eimunjeze said NAFDAC would continue to play its role in strengthening and regulating the pharmaceutical industry with an ultimate view to assuring drug security by improving the quality, safety and efficacy.